David Frick never planned to develop antiviral drugs. Instead he studied genetics in college,training with world-renowned scientists at Johns Hopkins University and Harvard Medical School. Then Frick’s body signaled an abrupt change of plans. Only months after finishing his Ph.D., his liver began to malfunction.
Video by Mary Rinzel
IN THIS VIDEO: David Frick gives a firsthand account of his own battle with hepatitis C and the grueling treatment that still drives his work today. View full size on YouTube
At the age of 26, he was diagnosed with the blood-borne hepatitis C virus (Hep C) – and cirrhosis of the liver, which often occurs after a long period of the infection. The postdoctoral researcher had contracted the virus through a blood transfusion he received just after birth.
“All that time, I didn’t think I was sick,” says Frick, an associate professor of chemistry, “because I never knew how it felt to be completely healthy.”
Now he learned he would not live long without a liver transplant.
Frick was lucky. Not only did he receive his new organ, but he also was cured of the virus by taking the available drugs, which typically did not work in transplant recipients. The drugs were also expensive, had toxic side effects and had to be taken for a year.
“The treatment makes you feel worse than the disease,” he says. “You are essentially giving yourself the flu with every shot of one drug, while the other drug makes you clinically depressed. It was the hardest year of my life, even harder to cope with than the transplant itself.”
Building better antivirals
Frick wanted to help others avoid having to go through his experience with the disease. So he ultimately decided to research development of better antiviral drugs, especially for Hep C.
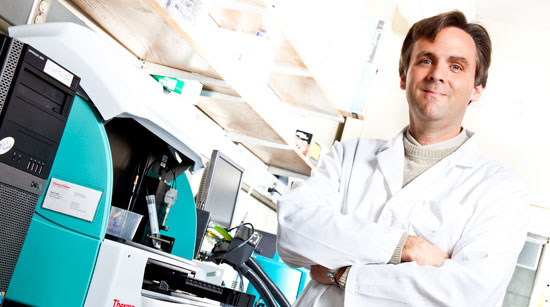
After his recovery, Frick built an antiviral lab from scratch. His goal was to find ways to shut off certain enzymes that viruses use to multiply inside human cells. Since he was new to the field, no elite research institute would take a chance on his ideas. So he started the project at a small medical school in New York with very little funding, while competing with established labs and every major pharmaceutical company.
After more than 10 years, Frick’s lab and its collaborators have found a new class of compounds that kills the virus in the host cell. Now the researchers are focused on understanding exactly how it works.
Although most people infected with Hep C don’t have many symptoms, long-term infection is the main cause of liver cancer and liver transplants. Hep C affects between 130 and 170 million people worldwide, and there is no vaccine.
“His line of inquiry into drug discovery for Hep C is now a hot area,” says Doug Stafford, director of UWM’s new Milwaukee Institute for Drug Discovery (MIDD). “It’s a billion-dollar opportunity. As of this summer, two pharmaceutical companies have gotten FDA approval for drugs that work in similar ways.”
Frick’s lab investigates an enzyme, helicase, which is made by the virus. Helicase “unzips” the viral RNA and maybe DNA of the cell it invades, so the virus can “read” genetic codes.
Blocking helicase stops the virus from multiplying in cells, and the Frick lab and its collaborators at the Scripps Research Institute in Florida and the University of Kansas have discovered the most potent helicase inhibitors to date.
Pharmaceutical companies have had little success in finding drugs that target helicase.
With funding from the National Institutes of Health and access to its molecular libraries, Frick’s team is searching one of the largest academic screening collections of bioactive chemicals in the U.S., looking for more helicase blockers to test.
A promising start

“We’ve screened more than 300,000 chemicals and found one that works well both in a test tube and in a cell,” says Frick. “We hope to develop this lead in preclinical trials with cells and animals. We still have a long way to go, but right now, we are the best-in-show for this drug target.”
The team also has a patent pending on the compound.
The long-term goal is to combine drugs that inhibit helicase with newly approved Hep C drugs so that the older drugs that cause the severe side effects are no longer needed. The newly approved medications are called protease inhibitors, and they function like drugs used to treat AIDS. Protease inhibitors, however, must be combined with older drugs, and those are the ones that make patients so sick.
A helicase inhibitor could be combined with the new protease inhibitors to stop the virus without use of the old drugs, making the treatment much easier on patients, he says.
Frick, who came to UWM from the New York Medical College last year, is one of four new biochemistry faculty hired to support MIDD. The addition increased the number of interdisciplinary MIDD-affiliated faculty on campus to 14.
After his liver transplant, Frick says he remembers feeling better immediately. Today, he is much more active than during his teens and 20s, enjoying activities like riding his bike to work in good weather – 18 miles round trip. He and wife Karyn, a neuroscientist and UWM professor of psychology, also keep up with two children, ages 6 and 4.







