A Career-Building Experience, an Affordable Degree
Get the best of both worlds: a college campus in a tree-lined neighborhood five minutes from Lake Michigan, and 10 minutes north of a bustling downtown with thousands of internships and job connections.
We are nationally recognized for our undergraduate research, and UWM students get real-world experiences that shape their education and careers, such as paid internships, entrepreneurship programs and community-based classes and volunteer opportunities. Forge your own path, your way, at UWM.
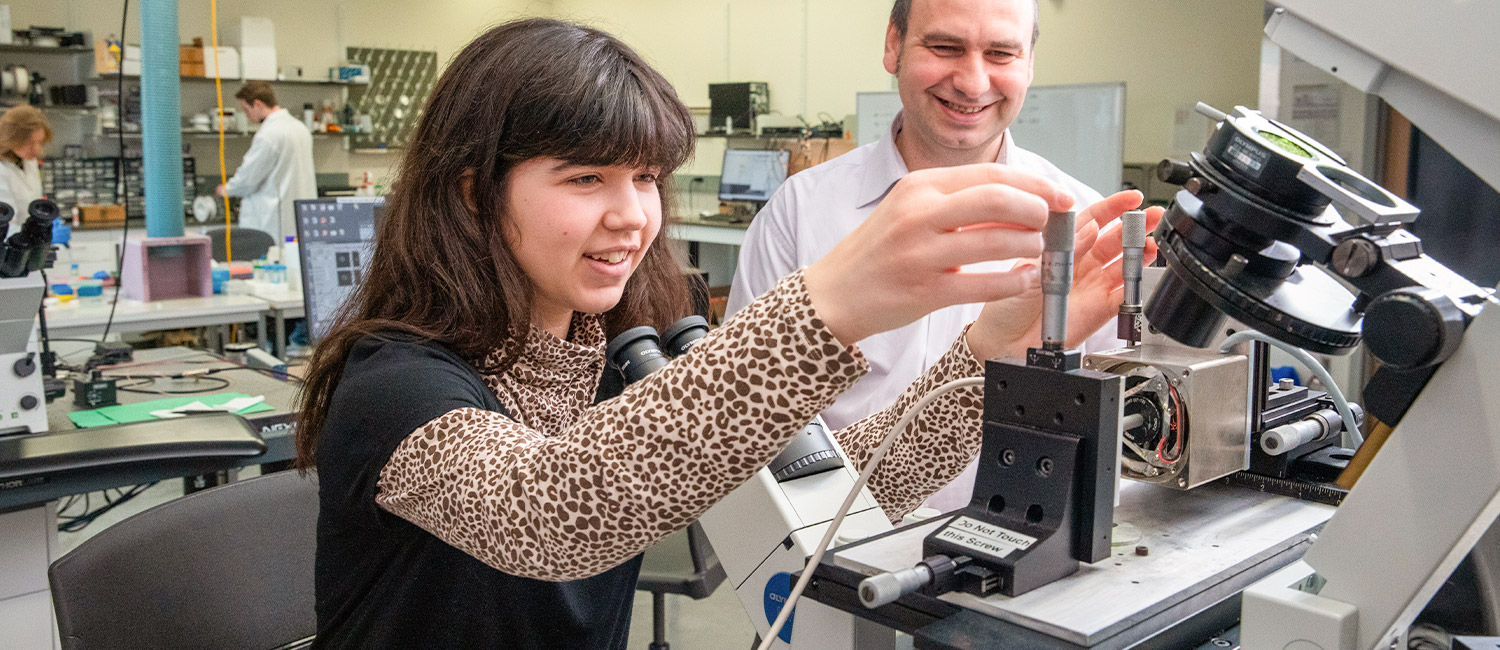
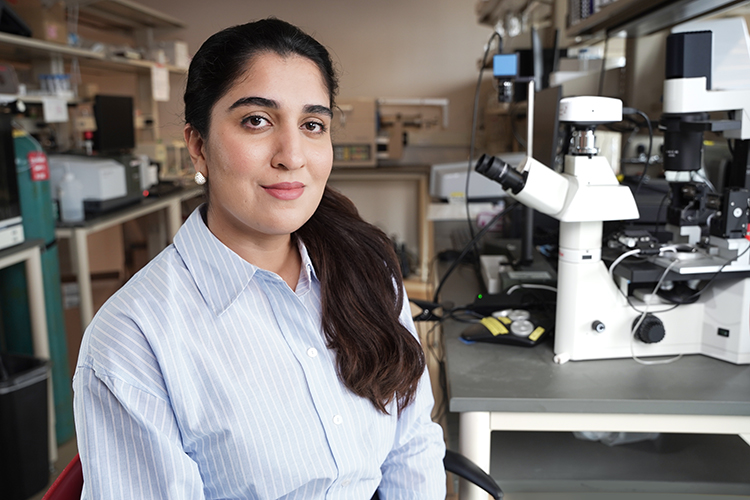
Learn by Doing
A well-rounded education doesn’t come from textbooks alone. We encourage all UWM students to build on what they learn in class with real-world experiences. Our students travel to other countries, do research, land internships, create startups, teach in Milwaukee classrooms, and more. No matter what you choose to study, you can get experience in your field before graduation day and leave UWM with a valuable degree and an impressive resume.
Your UWM Experience
Connect on ZeeMee
Meet and chat with other current and prospective UWM students.
Visit the Panther Family Portal
Stay informed and get connected in parent and family communities.
Support Services at UWM
You want your college journey to be fun, exciting and challenging. UW-Milwaukee is here to help you successfully navigate those challenges with a wide range of support services. Whether you’re looking to connect with internship opportunities, seeking an advisor who shares common ground, want help exploring major options or if you need basic medical services, you’ll find valuable support at UWM.
University Housing
UW-Milwaukee offers three university housing options for first-year students and up: Sandburg Hall, Cambridge Commons and RiverView. Upper-level UWM students have an additional campus housing option: Kenilworth Square.
All UWM residence halls have 24/7 security, fitness rooms, laundry access, utilities (including internet), regular social events and free shuttle service between the residence halls and UWM’s main campus.
Student Life at UWM
UWM students describe the university as being the best of both worlds. UWM’s campus is just five minutes from Lake Michigan and nestled in a safe, tree-lined neighborhood, so students get to enjoy the classic college experience. But if you want all the conveniences, job opportunities and excitement of a major city, UWM is also 10 minutes from Milwaukee’s bustling downtown.
On campus itself, you’ll find a welcoming, inclusive student community. There are always events happening around campus and with nearly 300 student clubs to explore, you’ll be able to form strong friendships.
UWM’s Impact
As a top-tier research university, we support groundbreaking work that helps real people and real communities.
We provide scholarships so that students have fewer roadblocks to success, and we offer entrepreneurship programs to help students in all disciplines develop the creativity and know-how to advance their careers. And a degree from UWM connects you with more than 218,000 successful alumni. You’ll find them in architecture firms, film studios, hospitals, classrooms, research labs, Fortune 500 companies and more.
“UWM has had a tremendous impact on my life. One of the things that impacted me most was studio life. The comradery, the extremely hard work, the late nights… It taught me grit, perseverance and those things that have allowed me to understand how to succeed in the rest of my career.”
Matt Rinka
Class of ’97
BS Architectural Studies

Main Campus
Our 104-acre main campus on Milwaukee’s east side is in a historic neighborhood just blocks from Lake Michigan. It is home to 21,931 graduate and undergraduate students.

Washington County Campus
UWM at Washington County sits on 87 acres surrounded by the beautiful Kettle Moraine State Forest. It serves 291 freshmen and sophomores.

Waukesha Campus
UWM at Waukesha occupies 86 acres on the western edge of the City of Waukesha. It serves 715 students in associate and bachelor’s programs.

UWM Online
UWM is home to Wisconsin’s top-ranked bachelor’s programs, as recognized by U.S. News & World Report. It offers 47 fully online degree and certificate programs.